An Orthogonal Approach To Antibiotic Discovery
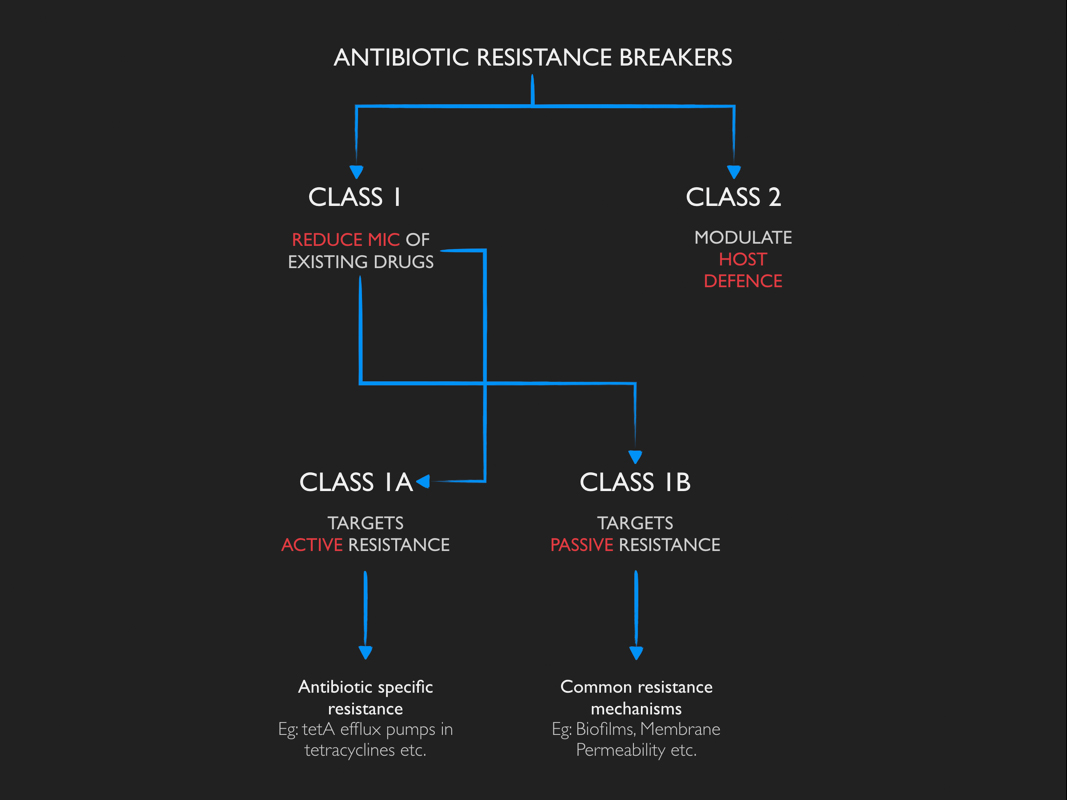
ARBs, sometimes referred to as antibiotic adjuvants, are non-antibiotic moieties which do not have any antimicrobial activity on its own, but, in combination with antibiotics enhance their antimicrobial activity and help overcome resistance barriers.
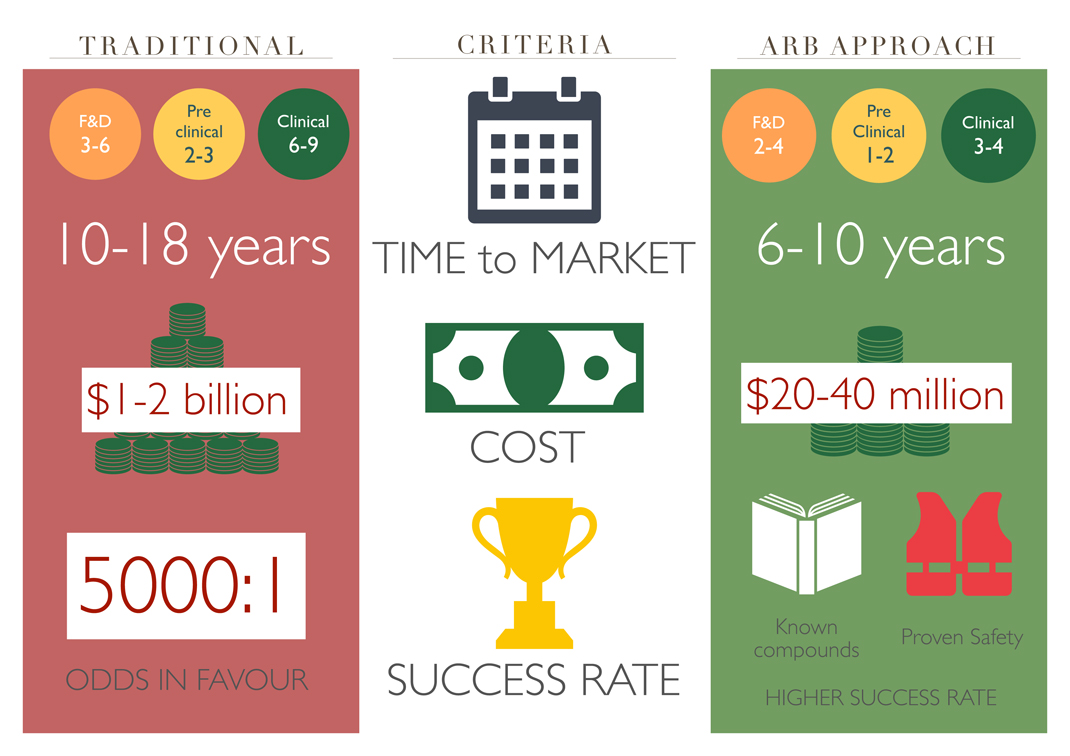
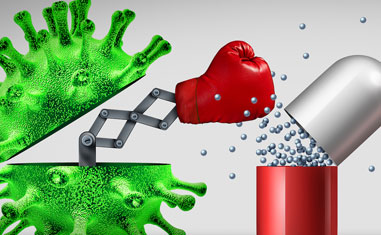
Traditional Vs ARB Approach
Repurposing drugs using ARBs overcomes many of the commercial barriers to developing new antibiotics and it is estimated that the use of ARBs could salvage many of the 200 or so existing antibiotics for the future generations.
Reasons to support the development of Antibiotic Resistance Breakers:
- Resistance to current antibiotics is rapidly increasing. Discovering new classes of antibiotics with novel mechanisms of action poses tremendous challenges as the scientific, commercial, and regulatory conditions are not presently aligned for the discovery of new drug classes
- ARBs can be combined with existing antibacterial agents with known pharmacological and toxicological effects, leading to considerable cost savings by eliminating much of the toxicological and pharmacokinetic assessments that would normally be required for the approval of a new drug or combination, thereby reducing the time to market
- ARBs would be particularly useful as their development could be faster, cheaper and provide a higher probability of success than that for new molecules
- If resistance develops to the first ARB combination, a second ARB could potentially rescue the same antibiotic. This cycle could be repeated many times, enabling old antibiotics to be used far into the future.
Trending Topics
DISCOVER OUR AREAS OF WORK
Genotoxicity studies
Genotoxicity studies can be defined as various in-vitro and in-vivo tests.
More
Cytotoxicity Study
Cytotoxicity is the quality of being toxic to cells which could be a chemical.
More
Gene Expression studies
Gene expression is a highly regulated mechanism that controls the function.
More